Knee Replacement Recovery Estimator
Personalize Your Recovery Plan
Answer a few quick questions to get your personalized pain estimates and recovery timeline.
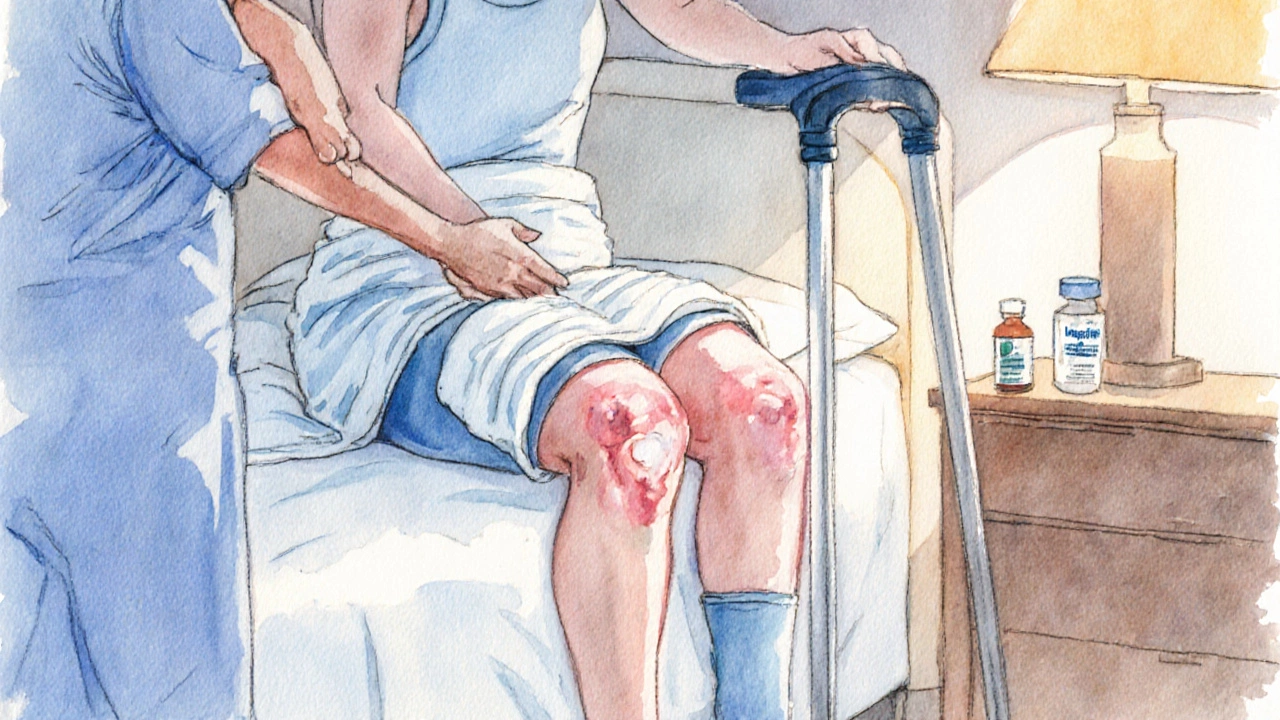
When you walk out of the operating theatre after a Knee replacement (also called total knee arthroplasty or TKA), the biggest question on most patients' minds is: "When will it get easier?" In reality, the first week is a roller‑coaster, and most people point to a single 24‑hour stretch that feels the toughest. Below we break down exactly when that day usually lands, why the body reacts that way, and what you can do to survive it with minimal agony.
Understanding the First‑Week Timeline
Right after surgery, your body launches three overlapping processes: pain management, inflammation control, and tissue healing. Each day brings a shift in the balance of those forces.
- Day 0 (the day of surgery): You’re under anesthesia, so you barely notice anything. The real story begins when the anesthetic wears off.
- Day 1 (the night after): Pain spikes as the nerve block fades. Swelling starts to appear, and you’ll likely be on a pain medication commonly opioids or NSAIDs prescribed by your surgeon.
- Day 2‑3: Physical therapy kicks in. You’ll attempt gentle knee bends and start walking with a walker or crutches.
- Day 4‑5: Swelling peaks, and muscles feel unusually weak.
- Day 6‑7: You begin to notice a slight dip in pain, though a lingering soreness can still be bothersome.
Most patients report that Day 2 is the hardest, but the exact answer varies with age, pain tolerance, and how closely you follow post‑op instructions.
Why Day 2 Is Often the Toughest
Three key factors converge on the second postoperative day:
- Inflammation the body’s natural response that causes swelling and heat around the surgical site typically reaches its peak.
- Pain medication wear‑off as the initial nerve block and high‑dose analgesics taper, you feel the raw surgical pain again.
- Early mobilization the first brisk PT session stresses the joint, testing the new implant and the surrounding soft tissue.
When those three pressures hit at once, the brain registers a sharp, stabbing ache that can feel worse than the incision itself. It’s also the moment when you start noticing how much the knee’s range of motion (ROM) is limited.
Typical Pain Levels by Day (Visual Guide)
| Day | Pain Rating (0‑10) | Typical Symptom |
|---|---|---|
| 0 (Surgery) | 0-2 (under anesthesia) | None, sleeping |
| 1 | 4-6 | Achy, sore, mild swelling |
| 2 | 6-8 | Peak inflammation, medication wear‑off |
| 3 | 5-7 | First PT session, bruising |
| 4 | 5-6 | Swelling peaks, still sore |
| 5 | 4-5 | Improved mobility, still tight |
| 6‑7 | 3-4 | Gradual decline in pain, more confidence walking |
How to Prepare for the Hardest Day
Knowing that Day 2 can be a pain peak gives you a chance to arm yourself with practical tactics.
- Pre‑emptive analgesia: Ask your surgeon about a peripheral nerve block that can be topped up on the first night. Adding a scheduled dose of acetaminophen and ibuprofen can smooth the transition when the block fades.
- Ice therapy: Apply a thin towel‑wrapped ice pack for 15‑20 minutes every two hours. Cold reduces cytokine activity, dialing down inflammation.
- Compression: Wear the elastic bandage or compression sleeve your clinic provides. It limits fluid buildup and improves venous return.
- Elevation: Keep the leg propped on pillows at least 12 inches above heart level while resting. Gravity‑assisted drainage cuts swelling.
- Deep‑breathing and gentle coughing: This prevents deep vein thrombosis (DVT) a clotting risk common after lower‑limb surgery and also keeps you oxygenated for better healing.
Doing these things before the second day rolls around can shave a point or two off that pain rating.
What to Expect During Physical Therapy on Day 2
Physical therapists will guide you through a series of gentle movements designed to protect the implant while restoring mobility.
- Quadriceps sets: Tighten the thigh muscle without moving the knee. Hold for five seconds, repeat 10‑15 times.
- Heel slides: Slowly slide the heel toward the buttocks, aiming for a 0‑30° bend.
- Ankle pumps: Flex and point the foot ten times to keep blood flowing.
The therapist may also assist you with a few assisted knee flexions using a continuous passive motion (CPM) machine. The CPM gently swings the joint back and forth, preventing scar tissue from locking the knee in place.
Red Flags: When “Hard” Is a Warning Sign
While a high pain score on Day 2 is normal, certain symptoms signal complications that need urgent attention.
- Sudden, intense swelling that spreads beyond the knee to the calf.
- Warmth or redness around the incision-possible infection.
- Sharp, shooting pain that doesn’t improve with medication-could be nerve irritation.
- Difficulty breathing or chest pain-rare, but may indicate a blood clot traveling to the lungs.
If any of these appear, call your surgeon or go to the emergency department right away.

Long‑Term Outlook: From Day 2 to Full Recovery
Getting past the toughest day is just the beginning. Here’s a quick snapshot of the typical milestones:
| Time Frame | What You’ll Usually Achieve |
|---|---|
| 2‑3 weeks | Walking unaided for short distances, climbing stairs with a handrail. |
| 6‑8 weeks | Full weight‑bearing, driving (if not on pain meds), light jogging for some. |
| 3‑6 months | Return to most recreational activities, stronger knee flexion (0‑110°). |
| 1 year+ | Implant durability peaks, patient‑reported outcomes comparable to healthy knees. |
Sticking to your rehab schedule and staying proactive about pain control will shrink that dreaded Day 2 hill and keep the rest of the climb manageable.
Quick‑Check Checklist for Day 2
- Take prescribed pain meds on schedule, no more than 4 hours apart.
- Ice for 15 minutes, then rest - repeat every 2 hours.
- Elevate leg above heart level while sleeping.
- Do the three PT exercises - 10 reps each.
- Walk with your assistive device for 5‑10 minutes, if cleared.
- Monitor swelling, temperature, and incision color.
Crossing each box off the list gives you a concrete sense of progress, even when the pain feels like a mountain.
Bottom Line
For most patients, **the hardest day after knee replacement lands on the second postoperative day** because inflammation, medication wear‑off, and the first burst of physical therapy collide. By preparing with pre‑emptive pain control, diligent icing, compression, and a focused PT routine, you can tame that spike and set the stage for a smoother, faster recovery.
When does pain usually peak after knee replacement?
Pain typically peaks on postoperative Day 2, when the nerve block fades and swelling reaches its highest level.
What can I do to reduce swelling on Day 2?
Apply ice for 15‑20 minutes every two hours, keep the leg elevated above heart level, and wear the compression sleeve provided by your surgeon.
Is it normal to feel sharp shooting pain on the second day?
Mild shooting sensations can occur as nerves adjust, but intense, unrelenting stabbing pain may signal a problem and should be evaluated by your surgeon.
Should I start walking on Day 2?
Yes, short, assisted walks (5‑10 minutes) are encouraged to improve circulation, as long as you stay within pain‑free limits and your doctor has cleared you.
When should I be concerned about infection?
Look for increasing redness, warmth, pus, or a fever above 101°F. If any appear, contact your surgeon immediately.









