Diabetes Medication Decision Tool
Which diabetes medication is right for you?
Based on your health conditions and goals, we'll show which class of medication (GLP-1 agonist or SGLT2 inhibitor) may be most beneficial for you.
Metformin has been the go-to pill for type 2 diabetes for over 60 years. It’s cheap, safe, and works for most people. But if you’ve been told recently that metformin isn’t right for you anymore, you’re not alone. More and more doctors are switching patients to newer drugs - not because metformin fails, but because these new options do more. They don’t just lower blood sugar. They protect your heart, help you lose weight, and even reduce the risk of kidney damage. So what’s replacing metformin? It’s not one drug. It’s a whole new class.
Why Metformin Isn’t Always Enough Anymore
Metformin works by making your liver less greedy. It stops it from dumping too much sugar into your blood. It also helps your muscles absorb glucose better. Simple. Effective. But here’s the catch: it doesn’t fix the root problem. Type 2 diabetes isn’t just about too much sugar in the blood. It’s about insulin resistance, chronic inflammation, and your pancreas slowly wearing out.
Many people on metformin still struggle with weight gain, high blood pressure, and rising A1C levels over time. Some can’t take it at all - stomach upset, diarrhea, or vitamin B12 deficiency make it unbearable. Others have kidney issues and can’t use it safely. That’s where the newer drugs come in.
The Two Main Replacements: GLP-1 Agonists and SGLT2 Inhibitors
There are two major classes of drugs now leading the shift away from metformin as the first-line treatment. Both are taken as pills or injections. Both have strong evidence backing them. And both are now recommended as first choices - even before metformin - for people with heart disease, kidney disease, or obesity.
GLP-1 receptor agonists (like semaglutide, liraglutide, dulaglutide) mimic a natural hormone your gut makes after eating. This hormone tells your pancreas to release insulin only when needed. It also slows digestion, so you feel full longer. The result? Better blood sugar control, weight loss of 10-15% on average, and up to a 26% lower risk of heart attack or stroke.
SGLT2 inhibitors (like empagliflozin, dapagliflozin, canagliflozin) work differently. They tell your kidneys to flush out extra sugar through urine. Sounds odd, right? But it’s brilliant. You lose sugar - and with it, calories. That’s why people lose 5-10 pounds on these drugs. More importantly, they reduce heart failure hospitalizations by 30% and slow kidney disease progression by up to 40%.
Real People, Real Results
Take Priya, 58, from Chennai. She was on metformin for 8 years. Her A1C stayed at 7.8%. She gained 12 kilos. Her blood pressure crept up. Her doctor switched her to semaglutide. Six months later, her A1C dropped to 6.1%. She lost 14 kilos. Her blood pressure normalized. She stopped taking three other pills.
Or Raj, 62, from Pune. He had early kidney damage from diabetes. Metformin was risky because his kidneys were declining. His doctor put him on empagliflozin. Within a year, his kidney function stabilized. His urine protein levels dropped. He didn’t lose much weight, but his heart got stronger.
These aren’t isolated cases. In 2024, the American Diabetes Association updated its guidelines to say: for patients with heart disease, chronic kidney disease, or obesity, start with a GLP-1 agonist or SGLT2 inhibitor - not metformin. The European Society of Cardiology says the same.

How Do These Drugs Compare?
Here’s how the top alternatives stack up against metformin and each other:
| Drug Class | How It Works | Weight Change | Heart Protection | Kidney Protection | Form | Common Side Effects |
|---|---|---|---|---|---|---|
| Metformin | Reduces liver sugar production | Neutral or slight loss | Mild benefit | No proven benefit | Tablet | Stomach upset, B12 deficiency |
| GLP-1 agonists | Boosts insulin, slows digestion | Loss of 10-15% | Strong benefit | Moderate benefit | Injection or tablet | Nausea, vomiting (usually temporary) |
| SGLT2 inhibitors | Removes sugar through urine | Loss of 5-10% | Strong benefit | Strong benefit | Tablet | Yeast infections, dehydration risk |
Notice something? Metformin doesn’t protect your heart or kidneys. The new drugs do. And they help you lose weight - something metformin barely touches. That’s why doctors are shifting.
Who Gets These New Drugs First?
These aren’t for everyone. But if you have any of these, you’re likely a strong candidate:
- You have heart disease, heart failure, or are at high risk
- You have chronic kidney disease (even early stage)
- You’re overweight or obese (BMI over 27)
- Your A1C stays high despite metformin
- You can’t tolerate metformin’s side effects
If you’re young, healthy, and your blood sugar is under control on metformin? Stick with it. There’s no need to switch. But if you’re struggling - with weight, energy, or complications - it’s time to ask your doctor about the alternatives.
What About Cost and Access?
Here’s the hard truth: these drugs are expensive. In the U.S., a month’s supply of semaglutide can cost over $1,000. In India, prices are lower but still steep - around ₹8,000 to ₹15,000 per month. Insurance often doesn’t cover them unless you have complications.
But that’s changing. Generic versions of SGLT2 inhibitors are now available in India. Dapagliflozin costs as little as ₹1,200/month. Some hospitals offer patient assistance programs. And with more local manufacturers entering the market, prices are expected to drop by 40-50% by 2026.
Don’t let cost stop you from asking. Talk to your doctor about options. Sometimes, switching from metformin to a cheaper SGLT2 inhibitor can reduce your total medication costs by cutting out other pills you’re taking for blood pressure or cholesterol.
What’s Next? The Future of Diabetes Care
The next wave is even more exciting. New drugs like retatrutide - a triple agonist that hits GLP-1, GIP, and glucagon receptors - are showing 25% weight loss in trials. Oral versions of GLP-1 drugs are now approved, so no more injections. And combination pills - like a single tablet with an SGLT2 inhibitor and a GLP-1 agonist - are coming to India by 2026.
This isn’t about replacing metformin because it’s bad. It’s about upgrading your treatment because we now have tools that don’t just manage diabetes - they reverse its damage.
Frequently Asked Questions
Is metformin being taken off the market?
No, metformin is not being taken off the market. It’s still widely used and recommended for many people, especially those who are healthy, lean, and have no heart or kidney issues. But for others - especially those with obesity, heart disease, or kidney problems - newer drugs are now preferred as the first choice. Metformin remains a solid backup option.
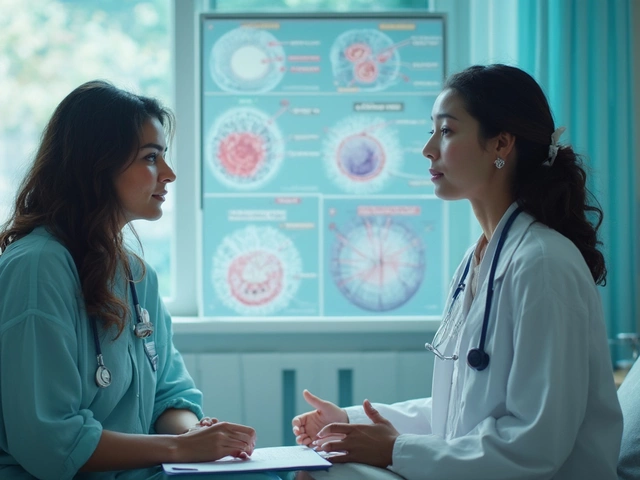
Can I switch from metformin to a new drug on my own?
No. Never stop or switch diabetes medications without medical supervision. These drugs can cause low blood sugar, dehydration, or kidney stress if not managed properly. Your doctor will check your kidney function, blood pressure, and overall health before making any change. They’ll also help you transition safely.
Do these new drugs cause weight loss in people without diabetes?
Yes. GLP-1 agonists like semaglutide and tirzepatide are now approved for weight loss in people without diabetes, under brand names like Wegovy and Zepbound. The same mechanism that lowers blood sugar also reduces appetite and slows digestion. This is why they’re so effective for weight management - whether or not you have diabetes.
Are there natural alternatives to these drugs?
There’s no natural supplement that replaces the proven effects of GLP-1 agonists or SGLT2 inhibitors. Berberine has some similar effects to metformin, but it’s not as strong or reliable. Lifestyle changes - diet, exercise, sleep - are essential and work best alongside medication. But they can’t replace these drugs if you need serious heart or kidney protection.
How long do I need to take these new drugs?
Diabetes is a lifelong condition. These drugs are meant to be taken long-term, just like metformin. Stopping them often leads to weight gain and rising blood sugar again. Think of them like blood pressure pills - you don’t stop taking them when you feel better. You keep taking them to stay protected.
What to Do Next
If you’re on metformin and not happy with your results - whether it’s weight gain, fatigue, or high A1C - ask your doctor about your options. Bring up GLP-1 agonists and SGLT2 inhibitors by name. Ask: "Is one of these right for me?" Show them your lab reports. Talk about your goals: losing weight? Protecting your heart? Avoiding kidney dialysis?
The goal isn’t just to lower your A1C. It’s to live longer, feel better, and avoid complications. The new drugs make that possible - for many, better than metformin ever could.