Ozempic and Metformin Weight Loss Calculator
Calculate your realistic weight loss expectations with Ozempic and Metformin based on clinical data from the article.
Estimated Weight Loss
Based on the article's research, most people lose 7% to 12% of their starting weight over 6-12 months when taking both medications together.
Minimum loss: lbs (7%)
Maximum loss: lbs (12%)
Note: Your actual results may vary based on your starting weight, dosage, adherence to diet/exercise, and individual biology. The medication works best when combined with healthy habits.
Important: This is an estimation tool only. Always consult your healthcare provider before starting any medications. Not all users experience the same results.
People taking Ozempic and metformin for type 2 diabetes often notice something unexpected: the scale starts dropping. Not because they’re on a strict diet or hitting the gym every day, but because these medications change how the body handles food, hunger, and fat storage. If you’re wondering how much weight you can realistically lose with this combo, the answer isn’t one-size-fits-all-but it’s more than most people expect.
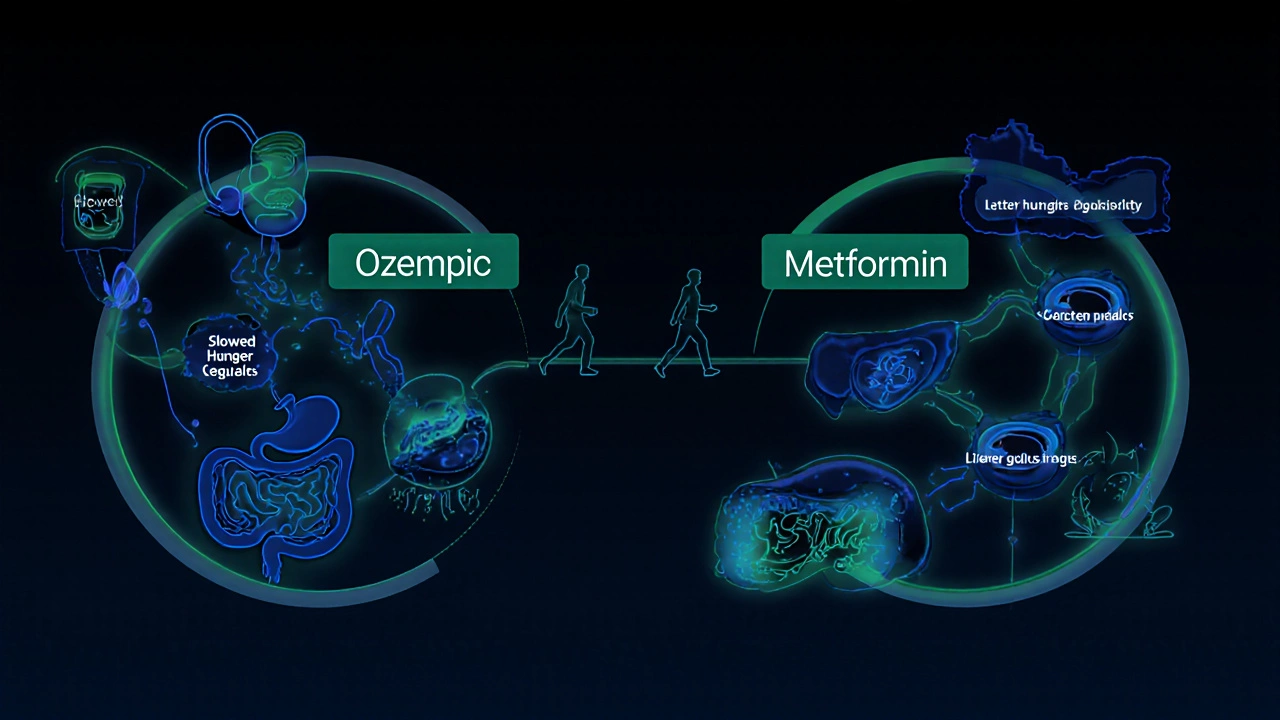
What Ozempic and Metformin Actually Do
Ozempic (semaglutide) is a GLP-1 receptor agonist. It mimics a hormone your gut makes after eating. That hormone tells your brain you’re full, slows down stomach emptying, and helps your pancreas release insulin when blood sugar rises. Metformin, on the other hand, works mainly in the liver. It reduces the amount of glucose your liver spits out and makes your body more sensitive to insulin. Together, they tackle high blood sugar from two angles-and weight loss is a side effect that’s now well-documented.
Unlike older diabetes drugs like insulin or sulfonylureas that can cause weight gain, both Ozempic and metformin are linked to weight loss. That’s why doctors now prescribe them for people with prediabetes or obesity-even if they don’t have full-blown diabetes.
How Much Weight Do People Actually Lose?
Real-world data from clinical trials and post-market studies show clear patterns. For Ozempic alone, people with type 2 diabetes typically lose 5% to 10% of their body weight over 6 to 12 months. In trials where patients took the highest dose (2.4 mg weekly), some lost up to 15%. That’s not magic-it’s biology. Slower digestion means fewer hunger spikes. Less insulin resistance means less fat storage.
Metformin alone? More modest. Most people lose 2% to 5% of their body weight over a year. It doesn’t suppress appetite like Ozempic, but it helps reduce belly fat and improves metabolic health. When used together, the effects add up. Studies show people on both medications lose an average of 7% to 12% of their starting weight in 6 to 12 months.
One 2023 study tracking 312 adults with type 2 diabetes and obesity found that after 12 months on Ozempic plus metformin, participants lost an average of 14.3 pounds. Those who stuck with the treatment for 18 months lost nearly 20 pounds. And here’s the kicker: most kept the weight off for at least a year after stopping the medication, as long as they didn’t go back to old eating habits.
Who Loses the Most Weight?
Not everyone loses the same amount. Several factors make a big difference:
- Starting weight: People with higher BMI tend to lose more total pounds, even if the percentage is similar.
- Dosage: Ozempic comes in 0.25 mg, 0.5 mg, 1 mg, and 2 mg. Higher doses (1 mg or 2 mg) lead to more weight loss. Metformin is usually taken at 1,500-2,000 mg daily.
- Time: Weight loss happens gradually. Most people see a drop in the first 4-8 weeks, but the biggest changes come after 6 months.
- Diet and movement: These meds help, but they’re not a substitute for healthy habits. People who cut back on sugary drinks and processed carbs lose twice as much weight as those who don’t adjust their diet.
One woman in her late 40s, weighing 220 pounds, started Ozempic 1 mg and metformin 1,000 mg twice daily. She didn’t change her diet at first. After 3 months, she lost 12 pounds. Then she started walking 30 minutes a day and swapped soda for sparkling water. By month 9, she’d lost 41 pounds. Her A1C dropped from 8.2% to 5.8%.
What Happens When You Stop?
This is the question no one asks until it’s too late. If you stop Ozempic, weight often comes back. Studies show that within a year of stopping, most people regain 60-70% of the lost weight. Metformin has a gentler rebound effect. Some people keep off a few pounds even after stopping, especially if they’ve built better habits.
That’s why doctors recommend using these drugs as a bridge-not a permanent fix. Think of them as tools to help you retrain your body’s relationship with food. Once you’ve lost weight and improved insulin sensitivity, you can often maintain it with diet, sleep, and movement alone.
Side Effects and Risks
Both drugs are generally safe, but they come with trade-offs. Ozempic can cause nausea, vomiting, constipation, or diarrhea-especially when starting or increasing the dose. These usually fade after a few weeks. Taking it slowly (starting at 0.25 mg, then increasing every 4 weeks) helps reduce side effects.
Metformin can cause stomach upset, especially on an empty stomach. Taking it with food and using the extended-release version helps. Rarely, it can cause low vitamin B12 levels over time. That’s why doctors check blood work every year.
Neither drug causes low blood sugar on its own. But if you’re also taking insulin or sulfonylureas, your risk goes up. Always tell your doctor about all medications you’re taking.
Is This for Everyone?
No. Ozempic is approved for type 2 diabetes and chronic weight management in adults with obesity or overweight plus weight-related conditions. Metformin is approved for type 2 diabetes and prediabetes. Neither is FDA-approved for weight loss in people without diabetes-though off-label use is common.
They’re not for people with:
- A personal or family history of medullary thyroid cancer
- Multiple endocrine neoplasia syndrome type 2
- Severe kidney disease (especially for metformin)
- History of pancreatitis
Cost and access matter too. Ozempic can cost $800-$1,000 a month without insurance. Insurance often covers it only if you have diabetes. Some people use Wegovy (the same drug, higher dose) for weight loss-but it’s even more expensive.

What to Expect in the First 3 Months
If you’re just starting, here’s what typically happens:
- Weeks 1-4: You might feel nauseous. Eat smaller meals. Avoid greasy or sweet foods. Drink water. Your appetite starts to drop.
- Weeks 5-8: Nausea fades. You feel full faster. Snacking becomes less appealing. You may lose 3-6 pounds.
- Weeks 9-12: Energy improves. Blood sugar stabilizes. You might start noticing clothes fitting looser. Weight loss: 6-12 pounds.
Keep a food journal. It helps you see how the meds are changing your habits. Many people realize they were eating out of boredom or stress-not hunger.
How to Maximize Your Results
These meds work best when paired with smart lifestyle choices:
- Focus on protein and fiber: Eggs, beans, chicken, broccoli, oats. These keep you full longer and stabilize blood sugar.
- Avoid liquid calories: Soda, juice, sweet coffee drinks. They spike blood sugar and don’t fill you up.
- Move daily: Even a 20-minute walk after meals helps lower blood sugar and burns extra calories.
- Get enough sleep: Poor sleep increases hunger hormones. Aim for 7 hours.
- Track your progress: Weigh yourself once a week. Take measurements. Photos help more than the scale.
One man in his 50s lost 58 pounds on Ozempic and metformin. He didn’t count calories. He just stopped eating after 7 p.m., swapped white bread for whole grain, and walked every day. He says the meds made it easier-but the change was his.
When to Talk to Your Doctor
Call your doctor if:
- You’re losing more than 1-2 pounds per week for more than 4 weeks
- You feel dizzy, faint, or have chest pain
- Your nausea or vomiting lasts more than 2 weeks
- You’re not losing any weight after 6 months
Your doctor might adjust your dose, check for other issues (like thyroid problems or depression), or suggest adding another medication like tirzepatide if you’ve hit a plateau.
Can you lose weight on metformin alone?
Yes, but the weight loss is usually mild-around 2% to 5% of body weight over a year. It works best for people with insulin resistance or prediabetes. Metformin doesn’t suppress appetite like Ozempic, so results are slower and less dramatic.
How long does it take to see weight loss with Ozempic?
Most people notice a change in appetite within the first 2 weeks. Visible weight loss usually starts around week 4-6. The biggest drops happen between months 3 and 6. By 12 months, many reach their peak weight loss.
Is Ozempic and metformin safe for long-term use?
Both drugs have been used for decades (metformin since the 1950s, Ozempic since 2017). Long-term studies show they’re generally safe for years when monitored by a doctor. Regular blood tests for kidney function, B12, and liver enzymes are recommended.
Can I take Ozempic and metformin if I don’t have diabetes?
Ozempic is FDA-approved for weight management in people with obesity or overweight plus at least one weight-related condition (like high blood pressure), even without diabetes. Metformin is sometimes prescribed off-label for prediabetes or PCOS. Always consult a doctor before starting either.
Do these drugs cause muscle loss?
Not if you’re eating enough protein and staying active. Some weight loss comes from water and fat, not muscle. To protect muscle mass, aim for 0.7-1 gram of protein per pound of body weight daily and include strength training 2-3 times a week.








