Post-Surgery Anger Risk Calculator
This tool assesses your risk of experiencing anger after open-heart surgery based on key factors discussed in the article. Enter your details below to see your personalized risk level.
Key Takeaways
- Anger after open‑heart surgery often stems from a mix of physiological, medication‑related, and psychological factors.
- Inflammation, hormonal shifts, and drugs such as beta‑blockers can directly affect mood.
- Pain, disrupted sleep, and ICU delirium amplify irritability.
- Practical coping tools include gentle breathing, journaling, cardiac rehab, and professional counseling.
- Seek medical help if anger is intense, persistent, or paired with thoughts of self‑harm.
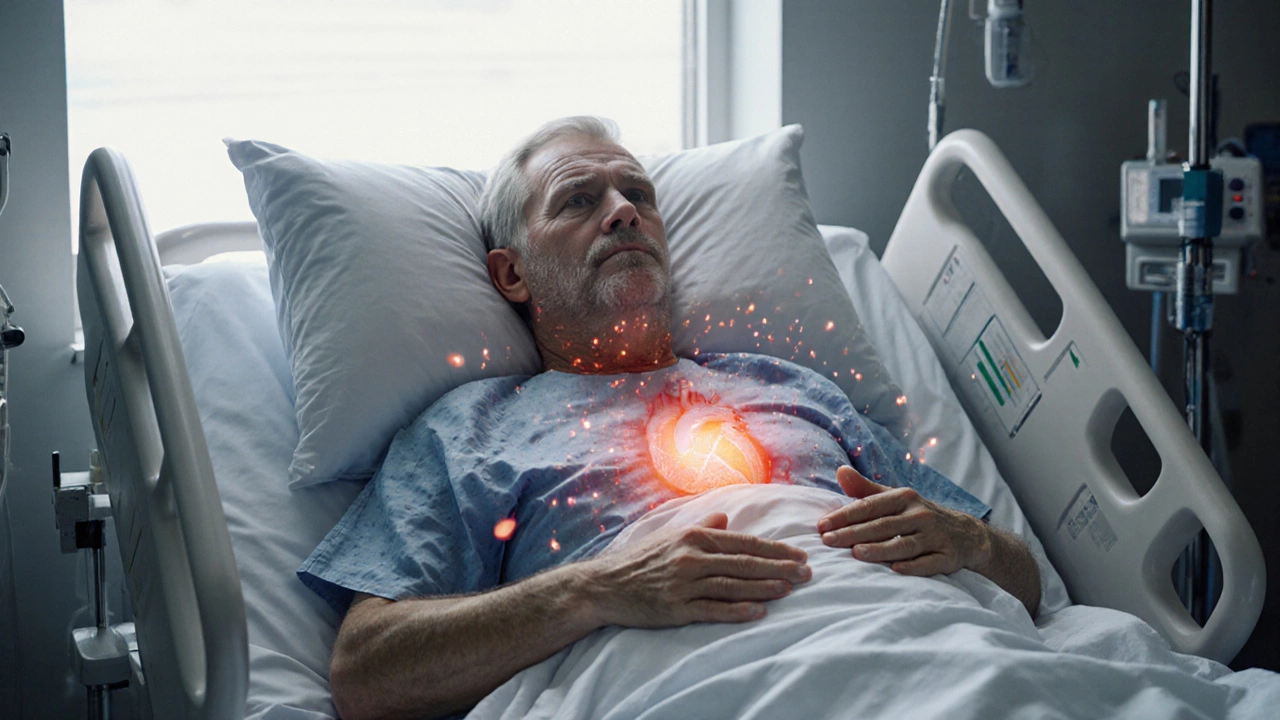
When you come out of open‑heart surgery a major cardiac operation that opens the chest to repair or replace heart structures, feeling angry isn’t rare. The body’s stress response, medication side‑effects, and the emotional shock of a life‑changing event all collide, creating a perfect storm of irritability. Below we break down why this happens and what you can do about it.
Physiological Triggers Behind Post‑Surgery Anger
After the chest is closed, the body launches a cascade of reactions to heal the wound. Two of the biggest contributors to mood swings are postoperative inflammation the swelling and immune activity that occur around the surgical site and hormonal imbalances.
Inflammation releases cytokines such as IL‑6 and TNF‑α. While essential for tissue repair, these proteins also act on the brain’s limbic system, the region that regulates emotions. Studies from leading cardiac centers in 2023 showed that patients with higher cytokine levels reported a 30% increase in irritability scores during the first two weeks after surgery.
At the same time, stress hormones like cortisol surge. Cortisol spikes are a normal "fight‑or‑flight" response, but prolonged elevation can blunt serotonin production, leaving you more prone to anger and frustration.
Medication Side‑Effects That Fuel Irritability
Doctors prescribe several drugs to keep the heart steady and the incision clean. Unfortunately, a few common classes have mood‑altering side‑effects.
| Medication | Primary Purpose | Typical Emotional Side‑Effect |
|---|---|---|
| Beta‑blockers Drugs that lower heart rate and blood pressure | Prevent arrhythmias | Fatigue, low mood, irritability |
| Steroids (e.g., prednisone) Anti‑inflammatory drugs used to reduce swelling | Control inflammation | Manic‑like energy swings, heightened anger |
| Opioid analgesics | Pain relief | Emotional lability, anxiety |
| Statins | Cholesterol management | Muscle aches, occasional mood dips |
It’s crucial to communicate any sudden mood changes to your cardiologist. Often, a simple dosage tweak or switching to a different class can ease the anger without compromising heart safety.
Psychological Stressors Unique to Cardiac Patients
Surviving a major operation forces you to confront mortality head‑on. The fear of another heart event, concerns about lifestyle limitations, and the sudden dependence on others can ignite anger as a defense mechanism.
Think of it as the mind’s way of saying, "I’m not ready to give up control." This emotional protest is normal, but if it lingers, it can become a barrier to recovery.
Many patients also struggle with identity shifts. A former runner who now needs to walk slowly may feel robbed of their former self, leading to resentment and short‑tempered outbursts.
Sleep Disruption, Pain, and ICU Delirium
Good sleep is a cornerstone of emotional balance. After postoperative pain the discomfort that follows surgical incision and chest tube removal, many patients experience fragmented sleep, nocturnal hypoxia, or the need for frequent medication dosing.
Sleep deprivation raises cortisol and reduces serotonin, both of which amplify anger. A 2022 sleep‑study of cardiac patients found that those sleeping less than five hours a night reported a 45% rise in irritability scores.
For those who spent time in the intensive care unit (ICU), delirium is another hidden culprit. ICU delirium blends confusion, visual hallucinations, and heightened emotional responses. Even after discharge, lingering cognitive fog can manifest as sudden outbursts.
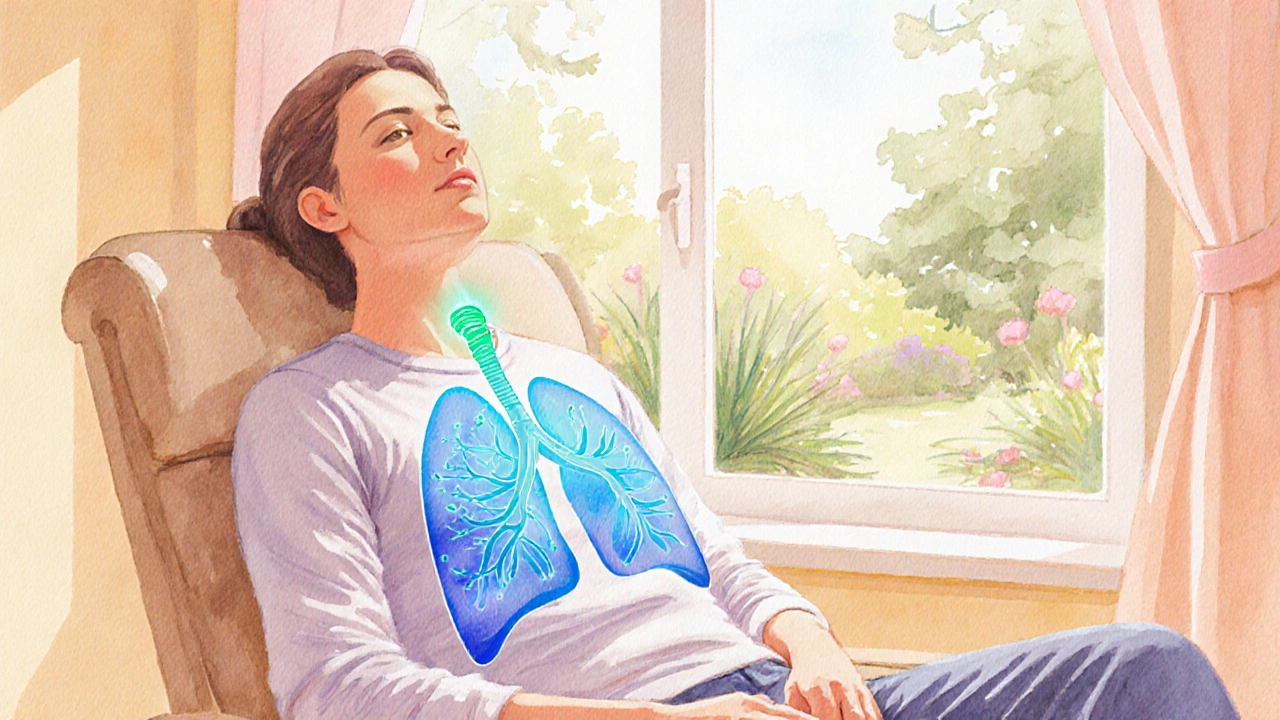
Practical Coping Strategies
- Breathing & Grounding: Practice 4‑7‑8 breathing (inhale 4seconds, hold 7, exhale 8). This simple technique lowers heart rate and tempers the fight‑or‑flight surge that fuels anger.
- Journaling: Write down what triggered your irritation. Naming the trigger reduces its power and helps you spot patterns.
- Cardiac Rehabilitation (cardiac rehab a supervised program of exercise, education, and counseling): Structured activity releases endorphins, improves sleep, and provides a supportive community.
- Gentle Exercise: Start with short walks, progressing as your surgeon permits. Physical movement counteracts the inflammation‑induced mood dip.
- Sleep Hygiene: Keep the bedroom cool, avoid screens an hour before bedtime, and use a white‑noise app if hospital noises linger.
- Medication Review: Schedule a follow‑up to discuss any mood side‑effects. Your doctor may replace a beta‑blocker with a different rhythm‑control drug.
- Professional Counseling: A therapist familiar with cardiac patients can teach cognitive‑behavioral tools to reframe fear and anger.

When to Seek Professional Help
If any of the following apply, reach out to your healthcare team promptly:
- Anger that feels uncontrollable or leads to aggression.
- Thoughts of self‑harm or hopelessness.
- Persistent insomnia (more than 7days) despite sleep hygiene.
- New or worsening chest pain, shortness of breath, or palpitations that coincide with mood spikes.
- Signs of ICU delirium lingering beyond two weeks (confusion, disorientation).
Early intervention prevents emotional distress from sabotaging your heart recovery and reduces the risk of long‑term depression.
Key Takeaway for Your Recovery Journey
The intense emotion you’re feeling right now is a natural response to major surgery, medication, and the upheaval of daily life. By understanding the underlying triggers-like post open-heart surgery anger-and applying targeted coping tools, you can regain emotional balance and support your heart’s healing process.
Frequently Asked Questions
Why do beta‑blockers make me irritable?
Beta‑blockers slow the heart and blunt adrenaline. While this protects the heart, it can also dampen the brain’s reward pathways, leading to low mood and irritability in some patients.
Can steroids really cause anger?
Yes. Steroids like prednisone raise glucose and affect neurotransmitter balance. Many patients report ‘mood swings’ or a sudden surge of anger, especially during the first two weeks of treatment.
Is it normal to feel angry when I’m still in the hospital?
Absolutely. The hospital environment-noises, limited privacy, and constant monitoring-can trigger frustration. Acknowledge the feeling, use breathing exercises, and speak with the care team about any discomfort.
How long does post‑surgery anger usually last?
For most patients, the intensity peaks in the first two weeks and gradually eases by the sixth week, especially with rehab and medication adjustments. If it persists beyond three months, a mental‑health evaluation is advised.
Can exercise help reduce my irritability?
Gentle aerobic activity boosts endorphins, improves sleep, and lowers inflammatory markers-all of which contribute to a calmer mood. Start with short, supervised walks and follow your cardiac rehab plan.